COVID-19 and essential NCDs care
20 August 2020 – The South Africa Non-Communicable Diseases Alliance (SA NCDs Alliance) is raising concern over the systemic neglect of non-communicable conditions (NCDs) like obesity, diabetes, high blood pressure, cancer, asthma and mental health problems due to neglected NCDs prevention and treatment. Download infographics
Dr Vicki Pinkney-Atkinson, Director of SA NCD Alliance says, “People living with NCDs believe it’s a health right to have proper access to care and medicines, especially now during a time of pandemic. Before COVID-19, the NCDs group of conditions killed most South Africans and remained neglected within government policy and budgets. For so long the many millions of people living with NCDs have lamented, ‘it would be better if I had HIV, then I would get access to quality care and medicines.”
NCDs, called underlying conditions during COVID-19, cause most deaths in South Africa. Diabetes kills more women than any other single illness for many years. (1) Government media acknowledge that 90% of those who die following COVID-19 infection had one or more NCD. (2)
The early figures coming out of Wuhan showed that NCDs increased the risk of complications and dying. It was clear that survival depended on well-managed conditions such as diabetes. It immediately exposed the fault lines in NCDs care.
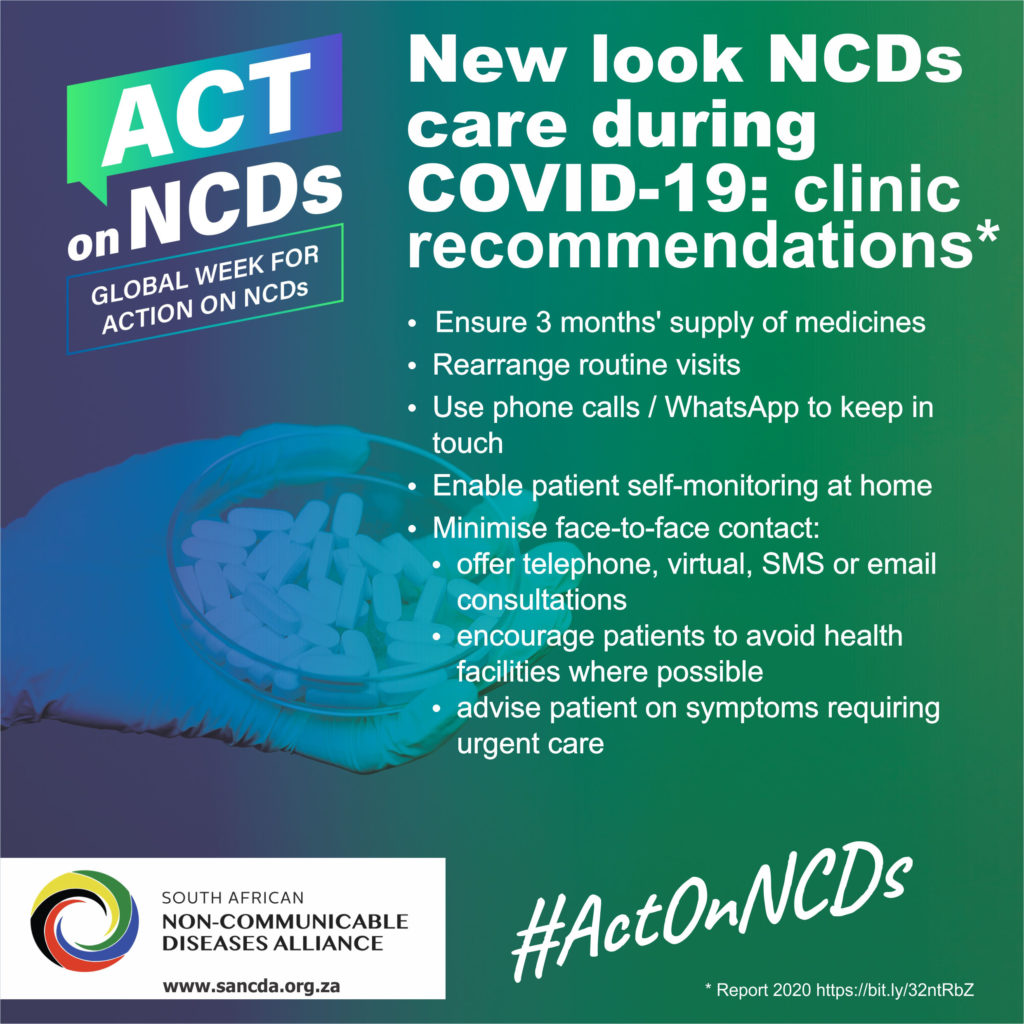
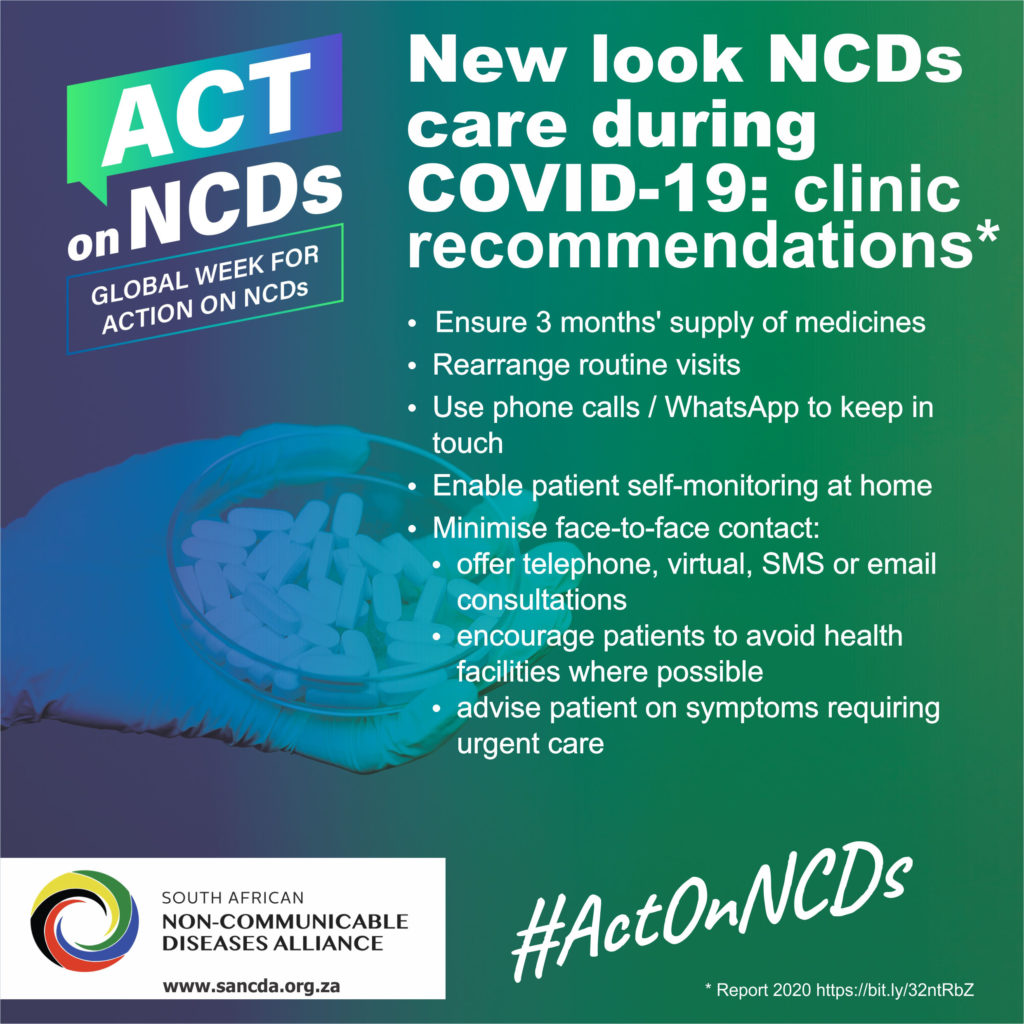
The aim is to get government to implement ongoing care for those living with NCDs by health workers during and beyond COVID-19. This includes ensuring adequate supply of medications that don’t involve travel and visits to facilities and making use of online and tools for consultations to minimise physical interaction and exposure.
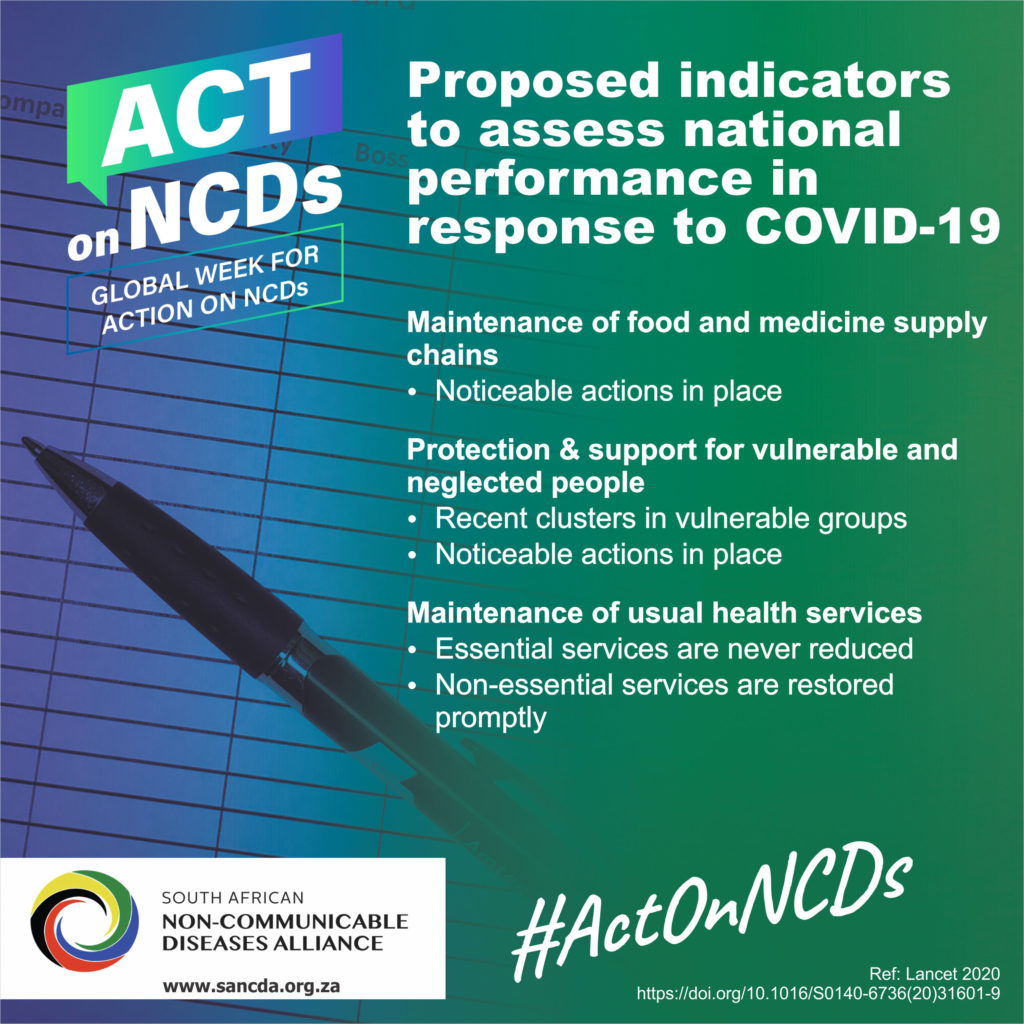
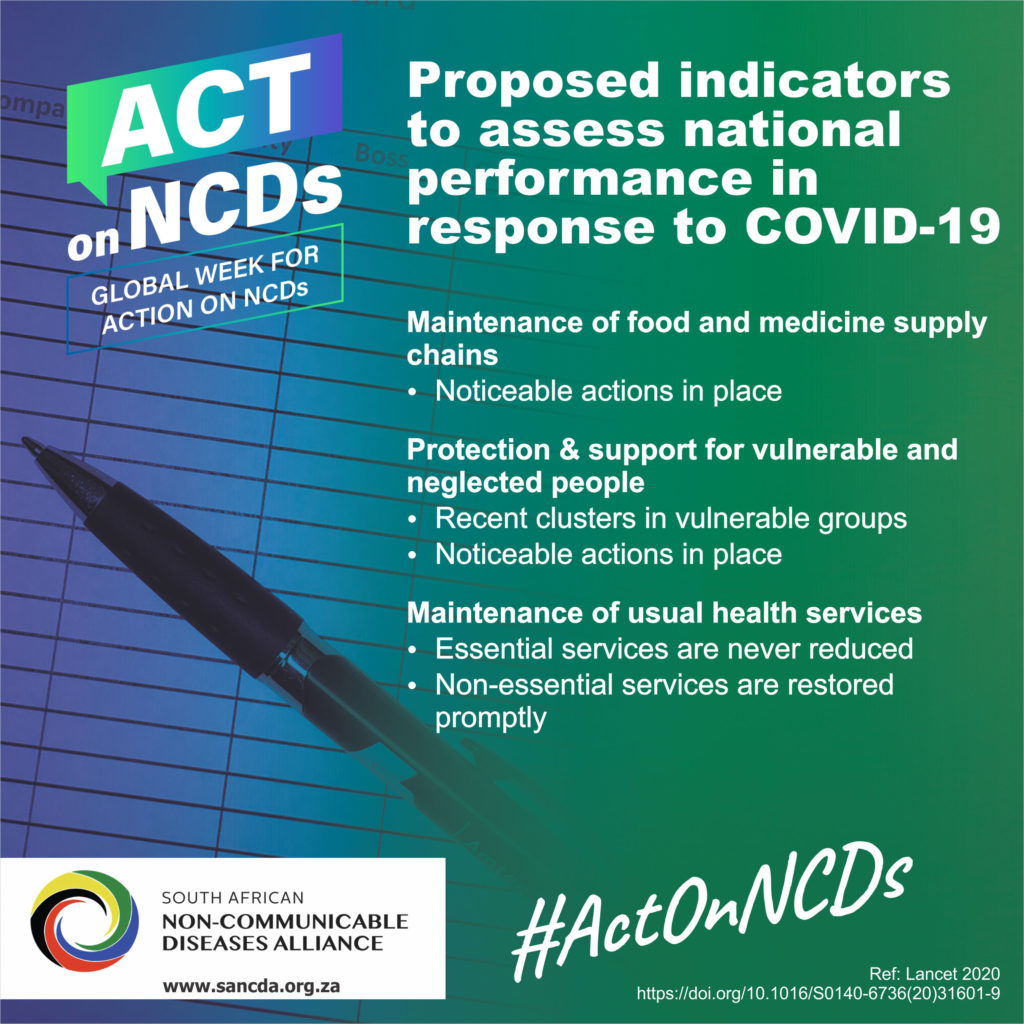
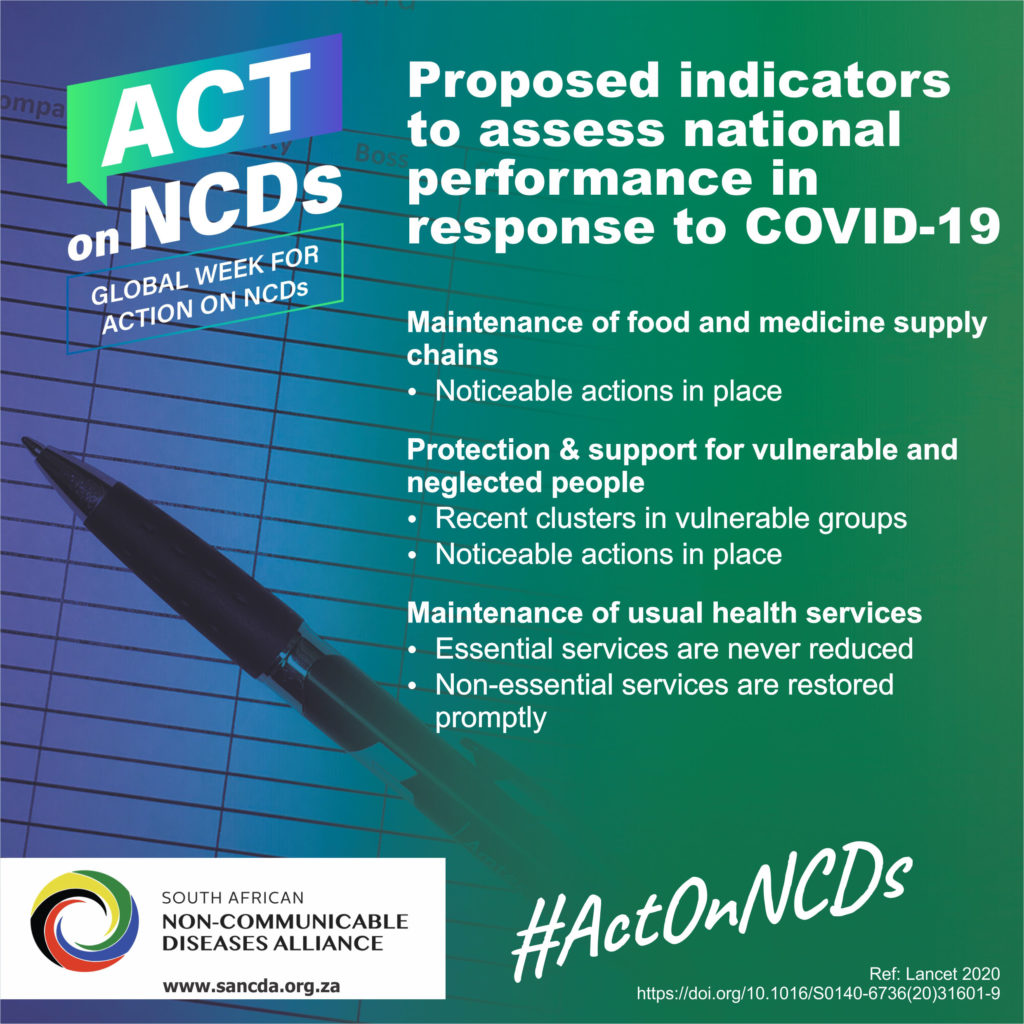
The Alliance further proposes performance indicators to assess government’s response to COVID-19 and ongoing NCDs care such as maintenance of food and medicine supply chains, protection and support for vulnerable and neglected people and maintenance of usual health services.
“As South Africans went into lockdown in March, the SA NCDs Alliance initiated online support, counselling and information services to keep people healthy such as the diabetes care line. Those of us living with diabetes soon learned that optimal blood sugar control is the best way to survive a COVID-19 infection. However, getting care and a regular supply of medicines in the public sector involved a stark choice; get your medications or get the virus. Unlike for HIV and TB, a remote non-clinic supply point is a rare option. Insulin, absolutely critical to sustain life in diabetes, is only available at a hospital-level even if there is a clinic next door,” elaborated Pinkney-Atkinson.
Zodwa Sithole, Head of Advocacy for CANSA added, “Patients are feeling frustrated and despondent as they struggle to access vital support services. A cancer patient’s low immunity and high infection risk for COVID-19, results in anxiety and physical distancing and hygiene measures add to a feeling of isolation even as lockdown levels are eased. Part of the response was the launch of our CANSA Tele Counselling service offering free, confidential cancer-related telephonic counselling available in seven languages.”
Nosipho (3) puts the human face on the access issue. In late pregnancy, she always needs insulin and asthma medication. Being a savvy diabetic, she knows she is at risk and tries to avoid the minimum five-hour round trip to get her insulin in central Cape Town during the COVID-19 surge. She knows that the risk of infection is high by using public transport and the long waiting lines at the hospital. When asked, the government sectors were unable to offer a solution.
For other NCDs like cancer, there are implications of delaying any screening that can result in cancers being detected at a later stage and affecting treatment outcomes.
Pinkney-Atkinson concludes, “What works to keep diabetics and other people living with NCDs safe, is not a mystery. There is plenty of evidence, we need action to provide ongoing NCDs care during COVID-19. (4) During the COVID-19 pandemic and beyond, we must go beyond stopping the virus and our right to get our ongoing essential services safely. We need these drugs and supplies (needles and syringes) to stay alive.”
For more information, please contact Dr Vicki Pinkney-Atkinson, Director of SA NCD Alliance at email [email protected]
Call 083 38 38-159. Alternate contact is Lucy Balona, Head: Marketing and Communication at CANSA at email [email protected].
Call 011 616 7662 or mobile 082 459 5230.
References:
(1) Statistics South Africa. Mortality and causes of death in South Africa, 2016: Findings from death notification [Internet]. Pretoria; 2018 [cited 2018 Mar 28]. Available from: http://www.statssa.gov.za/publications/P03093/P030932016.pdf
(2) SA Government News Agency. SA COVID-19 cases rise to 3 034. SANews.gov.za. 2020;2
(3) Not her real name
(4) Young T, Schoonees A, Lachman A, Kalula S, Mabweazara S, Musa E, et al. Taking stock of the evidence. Cape Town: Better Health Programme South Africa; 2020. 50 p
NCDs are a large group of health conditions that are generally not spread from person to person and used to be called chronic illness until 2000 when the Millennium Develop Goals force a new definition. Often the 5 main NCDs groups of conditions are noted: diabetes, circulatory disorders, mental health, cancer, and chronic respiratory illnesses. However, there are many more conditions that do not get a mention. Globally NCDs conditions are responsible for 41 million deaths annually and they are leading cause of death in South Africa since 2013. Diabetes is the leading cause of death of South African women.
However, the NCDs agenda is not just about illness it goes to a whole of society and whole of government response and for this we need an expanded understanding, meaning, NCDs+. The expanded NCDs+ advocacy agenda includes prevention, vulnerable populations, stigma control and disability. NCDs+ has many determinants (social, economic, and commercial) that disproportionately impact poor people. The Sustainable Development Goals (SDGs) address NCDs+ and its inclusion as an equal part of universal health coverage. (National Health Insurance in South Africa).
The SA NCDs Alliance, established in 7 years ago, is a civil society partnership between three trusted NCDs advocacy organisations: CANSA, Diabetes SA and the Heart & Stroke Foundation SA.
Its mission is for the people of South Africa have equitable access to quality NCDs+ prevention and management within universal health coverage/ NHI.
For this important COVID-19 and NCDs+ advocacy project nearly 90 civil society organisations are collaborating:
Cancer Alliance South Africa
Dementia South Africa
Epilepsy South Africa
Global Mental Health Peer Network
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) SA
National Kidney Foundation SA
Palliative Treatment for Children SA (PatchSA)
South African Disability Alliance
South African Federation for Mental Health
The SA NCDs Alliance’s goal in this programme it to ensure that the policy window of opportunity opened by the COVID-19 pandemic is used to make NCDs a priority in government policy through collaboration with NCDs civil society to put it on a par with HIV & TB. www.sancda.org.za
Diabetes helpline +27-81-578-6636
Summary: 1st WHO essential diagnostic list focusing on mainly communicable diseases with a recommendation to include more NCDs in a future edition. PHC and facility level essential package. Vicki Pinkney-Atkinson
Today, many people are unable to get tested for diseases because they cannot access diagnostic services. Many are incorrectly diagnosed. As a result, they do not receive the treatment they need and, in some cases, may actually receive the wrong treatment.
For example, an estimated 46% of adults with Type 2 diabetes worldwide are undiagnosed, risking serious health complications and higher health costs. Late diagnosis of infectious diseases such as HIV and TB increases the risk of spread and makes them more difficult to treat.
To address this gap, WHO today published its first Essential Diagnostics List (EDL), a catalogue of the tests needed to diagnose the most common conditions as well as a number of global priority diseases.
“An accurate diagnosis is the first step to getting effective treatment ….No one should suffer or die because of a lack of diagnostic services, or because the right tests were not available.”
Dr Tedros Adhanom Ghebreyesus, WHO Director-General.
The list concentrates on in vitro tests – i.e. tests of human specimens like blood and urine. It contains 113 products: 58 tests are listed for detection and diagnosis of a wide range of common conditions, providing an essential package that can form the basis for screening and management of patients. The remaining 55 tests are designed for the detection, diagnosis and monitoring of “priority” diseases such as HIV, TB, malaria, hepatitis B and C, human papillomavirus and syphilis.
Some of the tests are particularly suitable for PHC facilities, where laboratory services are often poorly resourced and sometimes non-existent; for example, tests that can rapidly diagnose a child for acute malaria or glucometers to test diabetes. These tests do not require electricity or trained personnel. Other tests are more sophisticated and therefore intended for larger medical facilities.
“Our aim is to provide a tool that can be useful to all countries, to test and treat better, but also to use health funds more efficiently by concentrating on the truly essential tests,” says Mariângela Simão, WHO Assistant Director-General for Access to Medicines, Vaccines and Pharmaceuticals. “Our other goal is to signal to countries and developers that the tests in the list must be of good quality, safe and affordable.”
For each category of test, the EDL specifies the type of test and intended use, format, and if appropriate for primary health care or for health facilities with laboratories. The list also provides links to WHO Guidelines or publications and, when available, to prequalified products.
Similar to the WHO Essential Medicines List, which has been in use for four decades, the EDL is intended to serve as a reference for countries to update or develop their own list of essential diagnostics. In order to truly benefit patients, national governments will need to ensure appropriate and quality-assured supplies, training of healthcare workers and safe use. To that end, WHO will provide support to countries as they adapt the list to the local context.
The EDL was developed following an extensive consultation within WHO and externally. The draft list was then considered for review by WHO’s Strategic Advisory Group of Experts on In-Vitro Diagnostics – a group of 19 experts with global representation. For more information see WHO website.
WHO will update the Essential Diagnostics List on a regular basis. In the coming months, WHO will issue a call for applications to add categories to the next edition. The list will expand significantly over the next few years, as it incorporates other important areas including antimicrobial resistance, emerging pathogens, neglected tropical diseases and additional NCDs.
 In a damning report by the South African Human Rights Commission (SAHRC) the KwaZulu-Natal Health Department and MEC Sibongiseni Dhlomo will have to answer why and how possibly thousands of Cancer patients have gone without treatment being left to die.
In a damning report by the South African Human Rights Commission (SAHRC) the KwaZulu-Natal Health Department and MEC Sibongiseni Dhlomo will have to answer why and how possibly thousands of Cancer patients have gone without treatment being left to die.
The report highlighted that in the province cancer patients have had to wait at least five months to see an oncologist. To further compound this they patients would have to wait another eight months after diagnosis before they can receive radiotherapy. Radiotherapy being the suggested treatment for patients suffering from cancer. Totaling over a year’s wait for treatment at thirteen months.
The problem stems from the Provincial department refusing to pay for a maintenance contract on two state of the art radiotherapy machines at Durban’s Addington Hospital. This caused and departure of senior oncologists from the hospital in protest to this refusal to pay for the upkeep of the R120-million machines.
These machines were instrumental in slashing those previously mentioned waiting times from five months to a mere two weeks. With a disease such as cancer time is of the essence to save lives and improve the patient’s quality of life. This is further backed up with international guidelines state that patients should receive treatment within 28 days of diagnosis.
The SAHRC has order in the report the department immediately repair both machines and remove the current backlog of patients waiting for care. This however, has no set time frame as the department has no oncologists left in Durban and only two remaining in Pietermaritzburg.
The report goes on further to say that the department knowing of the crisis and short fall of service had a duty to employ more staff and putting in place adequate screening, diagnosis and treatment of cancer patients. As well as an investigation into the health department be done by the Health Ombudsman and Premier Willies Mchunu into whether the Health MEC responded adequately to the matter in the short and long term.
The respondents in this matter were MEC Dhlomo, Addington Hospital, Inkosi Albert Luthuli Hospital (IALC) and the KwaZulu-Natal Department of Health, headed by Dr Sifiso Mtshali. The report states “The respondents have violated the rights of patients with cancer at the Addington and IALHC Hospitals to have access to health care services as a result of their failure to comply with applicable norms and standards set out in legislation and policies.”